Is your doctor’s report showing high creatinine levels in your blood giving you sleepless nights?
Don’t lose your sleep but take action to bring down the blood creatinine levels.
The foods you are consuming can be the culprit. Taking the right food is extremely important for you.
More so, foods can be your partner in managing creatinine levels, provided, you pick the right ones and avoid the ones that spike the creatinine levels up.
So, are you ready to learn which food reduces creatinine levels?
You will be happy to know that there are quite a few of them. To help you out, we have created a list of 6 food categories that bring down your creatinine levels.
Along with that, you will learn about what foods to avoid, and which lifestyle choices can help achieve your goal.
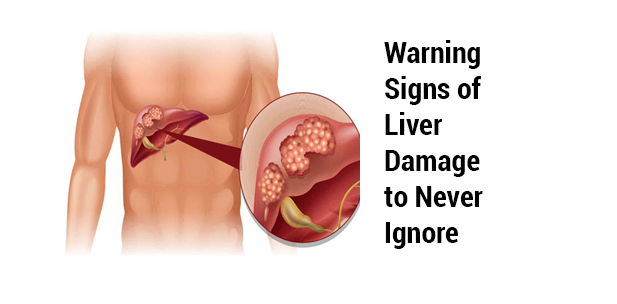
What is creatinine?
In a nutshell, creatinine is a waste that the body produces from protein digestion and natural muscle activities.
The kidney filters the blood and the waste ideally goes out of the body through the urinal route. If the kidney is not able to filter properly, the creatinine remains in the blood and is detected as high creatinine levels in the blood.
What are the causes of high creatinine levels?
There could be many reasons for high creatinine levels. The following are the most prevalent causes of high creatinine levels in the blood:
- Diseases such as High blood pressure and diabetes
- Kidney Inflammation and Infections
- Chronic Kidney disease
- Autoimmune diseases
- Certain Infections like HIV, Syphilis
- Hormonal issues like Thyroid
- Cancer
- Blockages in the Urinary tract and bladder
- Genetic which means family history
What are the symptoms of high creatinine levels?
When your blood creatinine levels are high, you might notice these symptoms:
- Your feet and ankles swell up
- Changes in how often you pee or the thickness of your pee
- Blood in your pee
- General Fatigue
- Your eyes look puffy
- Nausea and vomiting
- Cramps in your muscles
What is a normal creatinine level?
We have already told you that creatinine is a byproduct of the daily activities your muscles do. That’s the reason why men, women, and babies have differences in normal levels of creatinine.
Let us explain it to you, most women have lower levels of creatinine because they have less muscle mass than men. Check the list below to get an exact idea about the normal creatinine levels for men, women, and children.
- Women and older teenagers: 0.6 to 1.1 milligrams per deciliter (mg/dL)
- Men and some older teenagers: 0.8 to 1.3 mg/dL
- Babies: 0.2 mg/dL or higher
Understanding the normal levels of creatinine in your blood will help you take proactive steps when required, which include approaching a doctor and taking care of your diet.
Which Food reduces Creatinine Level?
Your diet plays an important role in bringing down your creatinine levels and focusing on it will help you get rid of the toxins and waste from your system. So, without wasting any more time, let’s check the foods that help reduce your creatinine levels.
Vegetables to reduce creatinine levels
These are some of the vegetables that can lower creatinine levels:
Cabbage
You should not forget cabbage as it is loaded with antioxidants and sulfur compounds. Even studies suggest that the antioxidants in it improve your kidney function.
Additionally, cabbage has dietary fiber that can boost digestion and clear your system of waste products and toxins, which includes creatinine.
Cauliflower
Cauliflower is another vegetable that is great for CKD (chronic Kidney disease).
It is also a vegetable that is high in fiber content and promotes the excretion of waste products from the body, including creatinine.
Besides fiber, cauliflower is a good source of antioxidants, vitamin C, and folate, which are excellent nutrients for kidney health.
You should also remember that cauliflower is low in potassium, which means it is good for people with kidney issues who need to manage their electrolyte levels.
Carrot
You must not miss carrots, as they have beta-carotene and pectins. a nutritious type of fiber. As per studies, pectin helps prevent kidney failure.
It has a diuretic effect that helps your kidneys get rid of water and toxins from your body. Pectin also reduces creatinine levels.
At the same time, you must note that though carrots are great for kidneys they are moderately high in oxalate.
So, if you have calcium oxalate kidney stones, you should have them in a small amount.
Onion
We all know that onion is a kitchen staple. But this everyday vegetable is good for your kidney health.
Especially, because onion contains allicin, a nutrient that helps improve kidney dysfunction and lower blood pressure.
Apart from that, onions are a good source of vitamin C, and calcium, which are important for maintaining healthy kidney function.
Onions are also rich in bioactive compounds that have antioxidant properties. These bioactive compounds are beneficial for you as an anti-inflammatory agent.
Eggplant
Eggplant or brinjal is another vegetable that may be part of your kitchen. But do you know that it is low in potassium and sodium?
That’s exactly why it is an excellent choice for those who have kidney disease.
A 2014 study indicated that chlorogenic acid, an antioxidant in eggplant, may decrease bad cholesterol and lower the risk of non-alcoholic fatty liver diseases. Another reason you should have this amazing vegetable.
Additionally, eggplant has diuretic properties which is good for your kidneys. It is rich in fiber which regulates your bowel movement and helps your body get rid of creatinine.
Soaked dark green leafy vegetables
Dark leafy green vegetables like spinach have nutrients, such as vitamins, minerals, and fibers. Most of them have antioxidants. But you need to have them after soaking them well overnight.
Doing so will help you maintain the levels of oxalates that cause kidney stones and reduce the kidneys’ power to filter wastes like creatinine.
Green leafy vegetables also have a high fiber content, which can help improve your digestion and promote regular bowel movements.
But you need to keep in mind that these vegetables are high in potassium, so those who are on a restricted diet and dialysis should not have them.
Fruits to reduce creatinine levels
If you are not taking fruits regularly, you are missing out on nutrients. Including some fruits in your diet can boost kidney health and reduce creatinine levels.
Cranberry is one such fruit that has some nutrients that are amazing for your kidneys.
Cranberries contain antioxidants like tannins and proanthocyanidins that protect your kidneys against oxidative damage and promote urine production.
When your urine production improves you easily filter waste like creatinine from your body.
Similarly, red grapes, blueberries, and raspberries have antioxidants that reduce inflammation and protect against kidney damage.
Apart from berries and grapes, melons, oranges, apples, pineapples, and cherries are rich in vitamins, minerals, and antioxidants, that support kidney health and reduce creatinine levels.
Add these fruits to your diet and their hydrating properties and nutrient content will help you keep your kidneys super healthy.
Seeds to reduce creatinine levels
Consumption of Seeds is another great way to improve your kidney health. You should add some pumpkin, chia, or flax seeds to your diet to boost kidney function.
Flaxseeds have antioxidant and anti-inflammatory properties, and as per experts, a dietary supplement of flaxseed oil reduces the chances of kidney failure.
Chia seed is a rich source of ALA (alpha-linolenic acid). It has great effects on kidney function.
Studies have also shown that pumpkin seeds improve blood sugar levels and reduce the risk of diabetic nephropathy, a common complication of diabetes that affects the kidneys.
These seeds have potassium and phosphorus, so the amount you can have each day depends completely on the type of dialysis you receive or your stage of kidney disease. We would advise you to consult your doctor in case of any doubt.
Whole Grains to reduce creatinine levels
A review of studies has shown that dietary fiber can help lower creatinine levels, and whole grains are rich sources of fiber.
Whole grains are an excellent source of antioxidants, dietary fiber, minerals, and vitamins.
Diets high in whole grains help improve kidney function if you have chronic kidney disease and lower the chances of developing such disease.
Whole grains have other health benefits too, like a lower risk of type 2 diabetes, and heart disease, lowered chances of obesity, and improved gut health. That’s why including whole grains in your diet is an excellent idea.
Plant-based proteins to reduce creatinine levels
Plant proteins contain calcium, magnesium, and vitamin C. Adding them to your diet can help reduce the acidity in your meals.
Reduction of acidity in meals can help improve kidney function.
So you can switch your animal protein sources with plant-based options, such as beans, lentils, and tofu.
Herbs to reduce creatinine levels
You should add the above-mentioned foods to your diet because it is an amazing way to reduce your creatinine level.
But if you want better results, you should take these Ayurvedic herbs to lower the high creatinine levels naturally and maintain the normal levels.
These herbs can shield your kidney from harm and help you lower creatinine levels. Moreover, the Ayurvedic herbs have no side effects.
Punarnava
Punarnava is beneficial for kidney health with diuretic and anti-inflammatory properties. It reduces the risk of inflammatory kidney conditions and helps remove kidney stones.
Kasni
Kasni is another herb that should be in your diet. It has diuretic properties and helps lower your creatinine levels.
Gokhru
If kidney stones are bothering you Gokhru is your go-to herb.
Gokhru improves your kidney health by preventing stone formation.
It breaks down existing stones and protects against kidney issues.
Makoye
Makoye promotes urine production and waste elimination.
Neem Chal
Neem chal has natural properties that lower creatinine levels; studies show that neem leaf protects the kidneys.
Peepal Chal
Peepal chal is believed to have diuretic properties that support kidney function.
You can find these herbs in Ayurvedic stores. You should definitely go for herbs that are organically grown for the best effects.
If you find difficulty finding these herbs, you can go for MedicoExperts’ Kidney Detox or Kidney Suddhi Kadha. This is one such supplement that has all the herbs mentioned above.
This is a perfect solution for your hectic lifestyle. You just need to mix it with hot water, keep it for 2 minutes, and have it and the herbs in this kadha will boost your kidney health.
What not to eat when you have high creatinine levels?
There are foods that you need to completely avoid when you have a high creatinine level.
- Restrict your sodium intake.
- Cut back on high-sodium foods like packaged items
- Avoid processed meats
- Avoid cheese
- Avoid fast food
- Avoid potassium-rich foods
Let’s have a look at some foods that you need to avoid in detail:
Potatoes
Potatoes are high in potassium and that’s why you need to avoid them if you have a high creatinine level. But you can reduce the high creatinine levels up to 20% if you first soak it in cold water for at least 5 minutes and then boil it properly.
Even then, if you have severe kidney conditions you should completely avoid potatoes.
Tomatoes
Tomato doesn’t fall on the kidney-friendly diet list because it is another fruit that is high in potassium. Apart from that, it is one of the fruits that have the highest levels of pesticides.
That’s why, you should completely avoid tomatoes if your creatinine level is high or you have a severe kidney problem.
Canned Food
From paneer to tuna, foods that are canned have sodium in a very high quantity. If you have CKD, you must avoid canned food totally, as your kidneys will not be able to filter the excess sodium like they normally do.
Drinks with Dark Colours
Most dark-coloured drinks have phosphorous to increase flavour and shelf life. Your body has a system to maintain the right balance of sodium but when you have CKD and other kidney-related problems that balance is disturbed.
Either your kidney works less effectively in this situation or your body tries to make the balance by changing hormone levels. This may affect your bones and heart health.
Because of this, you should avoid coloured drinks like sodas and other beverages.
Dairy Products
Dairy products are natural sources of potassium and phosphorous. Consuming too much dairy products along with phosphorous-rich food may impact your kidneys if you already have kidney issues.
Bananas
Bananas are high in potassium like potatoes. So, you should avoid them if you have high creatinine levels
Oranges
Oranges are rich in potassium. Even a small orange contains 174 mg of potassium. For the same reason, you should avoid orange juice and opt for beetroot juice or apple juice.
Dried Fruits
Dried fruits like apricots, prunes, raisins, and dates have high potassium and you should avoid them.
Pickles
Without pickle, your paratha may not taste that good but you should still avoid it if your creatinine levels are high.
Mostly because, while curing the pickle a huge amount of salt is used, which means they are high in sodium. Hence, you should avoid it.
Processed Meat
Chicken nuggets, popcorn, kebabs, paparonis and all other such meat packages you buy from the market are processed meat. These meats are salted, dried, and cured.
They have preservatives and high levels of sodium which are harmful to your kidney health.
Brown Rice
Brown rice has high potassium and phosphorus which makes it not suitable for those who have kidney issues.
Now that you know what foods to avoid, let’s learn about some home remedies.
Some other Home Remedies to lower creatinine levels
There is no doubt that diet plays a vital role in lowering your creatinine levels. But apart from that many other home remedies can help you bring the creatinine level down drastically.
- Avoid creatine supplements. These can increase creatinine levels in the body.
- Reduce protein Intake. Especially cut back on red meat, eggs, chicken, and dairy.
- Increase fibre consumption. Include whole grains, fruits, vegetables, and legumes in your diet.
- Limit Salt Intake. Processed foods are high in sodium, which can harm kidney function.
- Use NSAIDs Sparingly. Avoid overuse of non-steroidal anti-inflammatory drugs, especially with kidney disease.
- Quit smoking. Smoking can raise blood pressure and harm kidney function.
- Moderate alcohol consumption. Excessive alcohol can impair kidney function and raise blood pressure.
- Avoid Straining Exercises. Overuse of muscles can increase creatinine levels. So avoid exercises that strain you out.
Takeaway
A healthy diet low in salt and fat and rich in whole grains, fruits, and vegetables is the best if you have high creatinine levels.
The foods including vegetables, fruits, seeds, and whole grains mentioned in this article will help your body to naturally reduce creatinine levels.
Moreover, if you want better effects or if you are not able to create a routine to have these foods, you can add Ayurvedic natural herbs to your diet.
Along with that, you should consult a nephrologist without fail.
If you need any further help on foods, or herbs including how to find and buy organic herbs, or nephrologists, feel free to contact us.
Frequently Asked Questions (FAQs)
Q1. How can I lower my creatinine levels quickly?
1. Have a kidney-friendly diet mentioned in our article.
2. Avoid creatinine supplements
3. Lower your salt intake
4. Avoid smoking and alcohol
5. Avoid NSAIDs
Q2. Does lemon water reduce creatinine?
Q3. Which fruits can help reduce the creatinine levels?
Q4. Can I have chapati if I have high creatinine levels?
Q5. Does milk increase creatinine?
Q6. Which juice is best for the kidneys?
Q7. Is fasting good for creatinine?
Q8. Is curd good for creatinine levels?
Q9. Can coconut water help with creatinine?
Q10. How to lower creatinine overnight?
But that will be temporary and if you have severe kidney issues it may do more harm than good.
References
https://www.kidney.org/atoz/content/serum-blood-creatinine
https://bestpractice.bmj.com/topics/e
https://pubmed.ncbi.nlm.nih.gov/34974788/
https://www.nhs.uk/conditions/kidney-disease/#:~:text=Chronic%20kidney%20disease%20(CKD)%20is,or%20of%20south%20Asian%20origin.
https://kidneycop.com/are-carrots-and-cilantro-good-for-your-kidneys/#:~:text=In%20addition%20to%20beta%20carotene,and%20toxins%20from%20your%20body.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6341174/
https://onlinelibrary.wiley.com/doi/abs/10.1002/ptr.4751
https://www.kidney.org/atoz/content/leafy-green-vegetables
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8525749/#:~:text=In%20the%20kidney%2C%20flaxseed%20oil,chronic%20hemodialysis%20patients%20%5B20%5D.
https://pubmed.ncbi.nlm.nih.gov/20570704/
https://www.nature.com/articles/ejcn2014237
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-020-02079-y
https://pubmed.ncbi.nlm.nih.gov/31140512/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5409684/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4221362/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8941641/
Recommended Articles For You
- Which Food Reduces Creatinine Level: Top 6 of ThemIs your doctor’s report showing high creatinine levels in your … Continue reading Which Food Reduces Creatinine Level: Top 6 of Them
- What to Expect: Kidney Transplant Costs in IndiaAre you prepared for the financial impact of a kidney … Continue reading What to Expect: Kidney Transplant Costs in India
- Cost of Kidney Transplant in IndiaConsidering a kidney transplant? With 10% of the global population … Continue reading Cost of Kidney Transplant in India
- Creatinine Levels after Kidney TransplantCurious about your kidney’s post-transplant performance? Creatinine level after kidney … Continue reading Creatinine Levels after Kidney Transplant
- Best Hospitals for Kidney Transplant in IndiaTop 10 best hospital for kidney transplant in India 1.Fortis … Continue reading Best Hospitals for Kidney Transplant in India
- Eating the Right Diet After Kidney Transplant – GuidelinesDid you know that studies evaluating the dietary intake of … Continue reading Eating the Right Diet After Kidney Transplant – Guidelines
Recommendations to understand different treatments
Stem cell therapy for kidney failure in India to reverse chronic kidney disease
Do you think that healing damaged kidneys is next to impossible and the ominous shadow of chronic kidney disease looms large forever? If yes, you need to hear this out!…..
The news of end-stage kidney failure can be devastating not to mention stressful and painful. Regular hospital visits and constant medication can make life miserable and not sufficient anymore….
Next Logical Read
Medically Reviewed By MedicoExperts Editorial & Clinical Review Board on 09 May 2024