Does your child cough, choke, or struggle while eating?
Your child struggles with chewing and swallowing, and as a result, mealtime becomes stressful for you. This happens as your child may have dysphagia.
Dysphagia in cerebral palsy is a common condition. The reason behind this condition is that CP can affect the child’s muscles and coordination needed for swallowing and chewing. When the child cannot swallow, food or liquid may go down their airways to the lungs.
Due to discomfort, the child may avoid mealtime, and due to aspiration, there is a risk of infection in the chest or lungs. Avoiding food may lead to malnutrition.
But you may be relieved to know that dysphagia can be managed. Early detection, the right feeding therapies, and simple home adjustments can make your child’s swallowing safe and mealtime fun.
We will help you understand the signs and causes of dysphagia and also offer practical management options so that you can protect your child’s health and increase mealtime comfort.
Worried about choking, coughing, or repeated chest infections during meals? You don’t have to figure this out alone. Our specialists will guide you with safe, practical feeding solutions tailored to your child’s needs.
What Is Dysphagia in Cerebral Palsy?
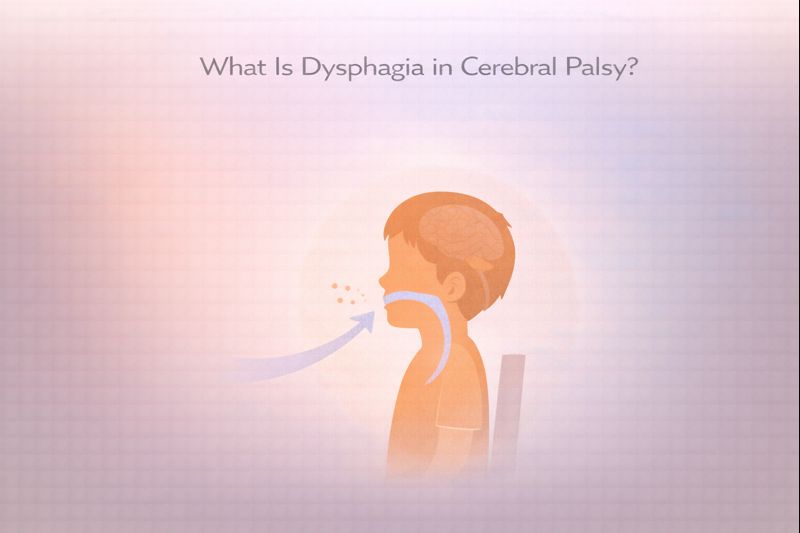
Due to dysphagia, the child has difficulty swallowing. Some children cannot coordinate the muscles of the tongue and the back of the throat. Others may have problems with the esophagus and difficulty moving food from the mouth to the stomach. This makes eating and drinking tiring, slow, uncomfortable and unsafe for the child.
Dysphagia in cerebral palsy happens because CP affects areas of the brain that control muscle movements and coordination. If these signals are weak or not coordinated, the child may struggle to chew properly or swallow at the right time.
This increases the risk of coughing and choking. Sometimes food may enter the windpipe, which can create a dangerous situation.
People may get confused between feeding difficulty and an eating disorder. But there is a difference between them. Feeding difficulties may include problems such as poor appetite, messy eating, or difficulty holding utensils.
Dysphagia, on the other hand, is a swallowing disorder where food or liquids may not move safely through the throat to the stomach.
Feeding difficulties can be stressful, but dysphagia can be dangerous for the child because it affects breathing, nutrition, and the child’s safety.
How Dysphagia Affects Feeding in Children with Cerebral Palsy?
These are some of the issues that children with cerebral palsy who have dysphagia face during eating or drinking anything:
Difficulty Chewing, Swallowing, and Coordinating Food
The child may struggle to manage food properly inside the mouth and throat. They may
- Find it difficult to chew food properly
- Face trouble moving food around the mouth
- Have delayed or uncoordinated swallowing
- Cough a lot or choke during meals
These challenges can increase the risk of food going down the wrong way.
Mealtime Stress for the Child and Parents
Your child feels uncomfortable and scared while eating; as a result, everyone around becomes worried and stressed, and this happens every day. These are the common mealtime events
- The child may feel frustrated or scared, or resist eating
- You and other family members may constantly worry about choking or aspiration
Instead of a bonding time for you and your family, it becomes the most worrisome and stressful time.
Impact on Nutrition, Growth, and Hydration
When the child has to fight with feeding difficulties every day, they may eat less or avoid some foods and liquids completely. And when they do it regularly, this can lead to poor weight gain, malnutrition, dehydration, low energy levels, and delayed growth.
These difficulties make early diagnosis and management of dysphagia even more important for your child. Managing it well will boost feeding safety, reduce stress, and support the healthy growth and development of your child.
Common Swallowing Problems in Cerebral Palsy
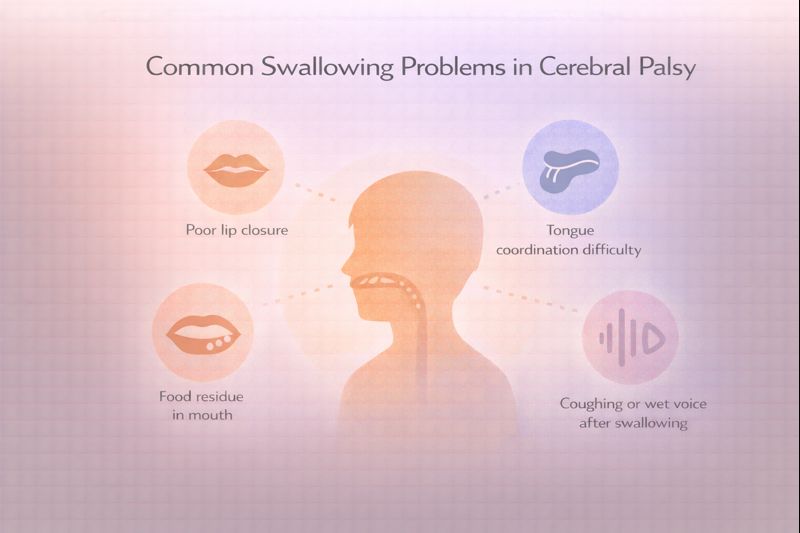
Here are the common issues related to swallowing that the child faces:
- The child may face poor lip closure, due to which they may struggle to keep their lips closed. As a result, they spill out their food or beverages. This can also make it hard to control them while chewing.
- Tongue thrusting is another issue that children with CP face. The tongue may push food forward instead of moving it toward the throat. This makes swallowing less efficient and can lead to gagging or food refusal.
- A delayed swallow reflex makes eating a complex process. The swallow may start later than it should, which allows food or liquid to pool in the mouth or throat and increases the risk of choking or aspiration.
- Coughing, gagging, or choking while eating or drinking are common issues that indicate that swallowing is not happening safely.
- Food may remain in the cheeks or on the tongue or feel stuck in the throat. This makes meals longer and more tiring for the child.
Causes of Dysphagia in Cerebral Palsy
Dysphagia may happen due to neurological damage in cerebral palsy. This damage affects motor control and coordination throughout the body of the child.
The brain injury that causes cerebral palsy hinders the complex communication system between the nervous system, which is required for safe and efficient swallowing. Many related factors lead to swallowing difficulties in children who have cerebral palsy.
Muscle Tone Abnormalities (Spasticity or Hypotonia)
Poor Oral-Motor Coordination
Weak Head, Neck, and Trunk Control
Sensory Processing Difficulties
Associated Neurological Damage
All of these problems can make swallowing difficulties worse and mealtimes more difficult and unsafe.
Signs of Dysphagia in Children with Cerebral Palsy
If your child has cerebral palsy, it’s important to watch for signs that indicate they might be facing trouble swallowing safely.
These warning signs can help you and the doctors identify problems early and offer support that gives your child comfort and safety. Here are the most common signs that a child may have dysphagia.
Frequent Coughing or Gagging During Feeding
Drooling or Food Leakage
Long Feeding Times
Recurrent Chest Infections
Poor Weight Gain
Refusal To Eat Certain Textures
Aspiration Risk in Cerebral Palsy: Why Dysphagia Can Be Dangerous?
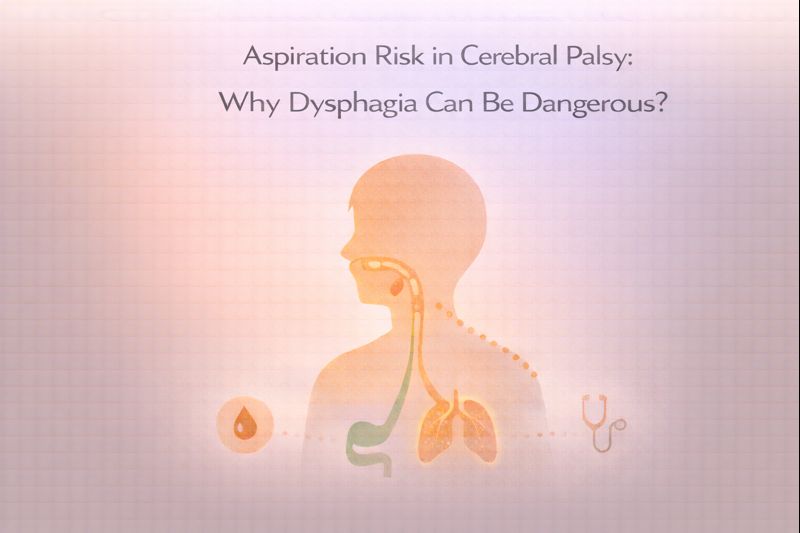
Dysphagia can make mealtimes dangerous. The biggest concern is something called aspiration, which happens when food, liquid, or even saliva goes down the wrong pipe into the lungs instead of the stomach.
That’s why it is important for you to understand aspiration and its risks, which can help you recognize when your child needs help and why getting treatment early is so important.
What is Aspiration?
When we swallow normally, a small flap called the epiglottis closes over our windpipe to keep food and liquid from going into our lungs. In children with dysphagia, this protective mechanism doesn’t always work properly.
Aspiration happens when something that should go to the stomach accidentally enters the airway and lungs instead.
This will help you understand it better: there are two tubes in the throat. One leads to the stomach (where food should go), and one leads to the lungs (where only air should go).
When the child cannot swallow properly, food or liquid can take the wrong path. Even small amounts of aspiration can be harmful for your child because the lungs aren’t designed to handle anything except air.
Signs of Silent Aspiration
Your child may aspirate without any sign, and that’s even more dangerous. This is called silent aspiration. You may be looking for coughing or choking as a sign when something goes into the lungs. But your child may not cough at all, even when food or liquid is going where it shouldn’t.
That’s why you should know these things about silent aspiration to keep your child away from danger:
- A wet or gurgly voice during or after eating
- Changes in breathing patterns during meals
- Seeming uncomfortable while eating for no clear reason
- Developing frequent chest infections without an obvious cough during meals
If you notice these signs, it’s important to get your child evaluated even if they’re not coughing.
Link Between Dysphagia and Pneumonia
When food, liquid, or saliva repeatedly enters the lungs, bacteria also enter there with these particles. This makes the lungs irritated and infected, which in turn can lead to pneumonia.
This is called aspiration pneumonia, and it’s one of the most serious complications of dysphagia. If your child aspirates, they may get pneumonia over and over again. It happens several times a year, sometimes.
Too many infections happening again and again can make your child very sick with fever, difficulty breathing, and fatigue. They can cause lasting damage to their lungs and make breathing problems worse over time. Aspiration pneumonia can even be life-threatening in severe cases.
Hence, preventing aspiration is an important part of managing dysphagia for your child’s health.
Why Early Management Is Critical?
You need to catch and treat swallowing problems early to ensure your child’s health and comfort. To do so, dysphagia needs to be identified sooner, so that a team of specialists can put safety measures in place to protect your child’s lungs.
These are some of the measures that can be recommended by the doctors: changing food textures, adjusting feeding positions, learning special techniques, or sometimes using alternative feeding methods.
Early intervention can prevent the chances of aspiration pneumonia in your child and help them maintain their nutritional needs
So, don’t wait and ignore the signs. Talk to your child’s doctor or talk to a speech therapist who specializes in swallowing.
How Dysphagia is Diagnosed in Children with CP?
Diagnosis of dysphagia in children with cerebral palsy needs a holistic approach that uses clinical observation with specialized testing. The diagnostic process starts when you notice signs like coughing during meals, increasing feeding times, or repeated respiratory infections.
Clinical Feeding Assessment
Swallow Evaluation by Speech Therapist
Instrumental Tests
Importance of Early Diagnosis
Early diagnosis transforms a potentially dangerous situation into a manageable condition, giving children with CP the best possible chance to thrive.
Management of Dysphagia in Cerebral Palsy
Managing dysphagia in cerebral palsy needs a personalized approach for each child’s specific needs and abilities. The goal of the management is to make eating safer, more efficient, and more enjoyable for your child. The aim is also to ensure adequate nutrition and prevent complications during eating and drinking.
Feeding Therapy for Dysphagia in Cerebral Palsy
Oral Motor Exercises for Swallowing
Diet and Texture Modifications
Safe Feeding Positions
These management strategies work together to create a comprehensive approach that prioritizes safety while supporting the child’s nutritional needs and development. Every child’s plan is unique and should be regularly reassessed as their needs change over time.
Early guidance can prevent serious complications like aspiration and poor nutrition. A professional feeding and swallowing evaluation can help identify risks and create a safer feeding plan for your child.
How Parents Can Support a Child with Dysphagia at Home?
You have an essential role as a parent in managing dysphagia daily. Your child’s healthcare team provides guidance and expertise, but it’s families who implement feeding strategies during every meal and snack.
Creating a supportive home environment and following recommended techniques can make a significant difference in both safety and success.
Safe Feeding Environment
Establishing the right setting for meals helps minimize distractions and reduces the risk of swallowing problems:
- You need to minimize distractions. Turn off the television, put away toys, and reduce background noise so the child can focus entirely on eating
- Proper lighting is important while eating. Ensure the feeding area is well-lit so you can clearly see the child’s face and watch for any signs of difficulty
- Arrange an appropriate seating. Use supportive chairs or adaptive equipment that keep the child in the correct position throughout the meal
- Have emergency supplies ready. Keep a suction device nearby if recommended by your medical team, and know how to respond if choking occurs
- Create a calm atmosphere during mealtime. Create a relaxed, positive environment where mealtimes feel safe rather than stressful
- Stay attentive to your child. Never leave a child with dysphagia unattended during meals
Slow, Calm Feeding Routines
Rushing through meals increases the risk of aspiration and makes eating more difficult for children with swallowing challenges:
- Offer small bites or sips. Give manageable amounts that the child can safely control, usually about half a teaspoon at a time.
- Wait between bites. Allow the child to fully swallow and clear their mouth before offering more food.
- Watch for signs of readiness. Let the child set the pace and look for cues that they’re ready for the next bite.
- Avoid pressure or forcing while eating. Never force a child to eat if they’re showing signs of distress, fatigue, or refusal.
- Take a break. There should be rest periods during longer meals to prevent exhaustion.
- Stay calm and patient. Your relaxed demeanor helps the child feel secure and reduces mealtime anxiety.
- Make the mealtime enjoyable. Even with necessary precautions, try to keep meals pleasant social times
Observing and Tracking Symptoms
Careful monitoring helps you recognize problems early and provides valuable information to your healthcare team:
- Watch for warning signs during meals, like coughing, choking, gagging, watery eyes, or changes in breathing
- Monitor after eating and note any wet or gurgly voice quality, which can indicate material in the throat
- Track respiratory symptoms and keep records of any fevers, congestion, or respiratory infections that might be related to aspiration
- Document feeding times and note how long meals take and whether the child seems more or less fatigued
- Record what works and keep track of which foods, textures, and techniques are most successful
- Monitor the child’s growth. Regular weight checks help ensure the child is getting adequate nutrition
- Keep a feeding diary of your child. Write down observations to share with therapists and doctors at appointments
Working with Therapists Consistently
The most successful outcomes happen when families partner closely with their healthcare team:
- Attend all therapy appointments. Regular sessions allow therapists to monitor progress and adjust strategies
- Practice recommended exercises. Do oral motor exercises and feeding techniques as prescribed, not just during therapy sessions
- Ask questions. Don’t hesitate to clarify instructions or express concerns about any recommendations
- Report changes promptly. Let therapists know right away if you notice new difficulties or improvements
- Follow the feeding plan. Stick to recommended food textures, liquid consistencies, and positioning guidelines
- Be honest about challenges. If something isn’t working at home, share this so adjustments can be made
- Stay educated. Learn as much as you can about your child’s specific type of dysphagia and management strategies
- Connect with other families. Support groups can provide practical tips and emotional support from those who understand
Supporting your child at home needs your dedication, patience, and vigilance. By implementing these strategies consistently, you can help your children eat more safely and comfortably.
Takeaway: Early Recognition Improves Safety and Quality of Life
Dysphagia in cerebral palsy is manageable, and you can make a real difference in your child’s life starting today.
Your child needs the right support to make their mealtime safe and comfortable. And you will be able to offer help to them when you are equipped with the right knowledge and a team of specialists by your side.
So if you see warning signs like coughing during meals, frequent chest infections, or poor weight gain, don’t wait because early diagnosis through proper swallowing evaluation can prevent serious complications like aspiration pneumonia and malnutrition.
Ready to take the next step. Connect with our specialists who understand dysphagia. Our team will help you create personalized feeding plan that keeps your child safe, well-nourished, and thriving.
Frequently Asked Questions (FAQs):
Q1. When to worry about swallowing problems in CP?
A. You should worry about swallowing problems in cerebral palsy if a child frequently coughs, chokes, or struggles while eating or drinking. Recurrent chest infections, poor weight gain, or very long feeding times are signs to seek medical advice.
Q2. Can dysphagia in cerebral palsy improve with age or therapy?
A. Yes, dysphagia can improve with the right feeding therapy, posture support, and diet modifications, especially when started early. While CP itself does not go away, many children learn to swallow more safely over time.
Q3. Is dysphagia common in all types of cerebral palsy or only in severe cases?
A. Dysphagia is more common in children with moderate to severe cerebral palsy, but it can also occur in milder forms. Even children who seem to eat well should be monitored for subtle swallowing problems.
Q4. How do I know if my child is aspirating silently?
A. Silent aspiration may not cause coughing or choking during meals. So you need to know these signs: a wet or gurgly voice, frequent chest infections, breathing changes during feeding, or unexplained fevers.
Q5. How long does feeding therapy take to show improvement?
A. Some children show small improvements within a few weeks, while others may need several months of consistent therapy. Your child’s progress depends on their condition, therapy frequency, and home practice.
References
Relevant Articles For You
Is Cerebral Palsy Curable?
Is cerebral palsy curable? This is the first and most urgent question parents ask after a diagnosis. The honest answer is that…..Read More
Speech Delay in Cerebral Palsy
Speech delay in cerebral palsy is one of the first challenges that makes you worried about your child’s future. When you…..Read More
Recommendations To Understand Different Treatments
Stem Cell Therapy for CP
Stem cell therapy lessens the symptoms, prevents complications in the future, and maximizes the independence of…..Read More
Combination Therapy for CP
Cerebral palsy affects movement, muscle tone, and coordination. Relying on a single therapy often falls short because…..Read More
Homeopathy for CP
Homeopathy is a system of medicine that stimulates the body’s innate healing mechanisms using diluted natural substances. It’s built on…..Read More
Ayurveda for CP
In Ayurveda, CP is linked to an imbalance in the Vata dosha, which governs movement and coordination. When Vata is out of…..Read More
Medically Reviewed by MedicoExperts Editorial & Clinical Review Board on 29 December 2025
Medical Disclaimer: This content is for informational purposes only and is not intended as medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider regarding any medical condition or dietary needs.