Do you know that youngsters in their prime and productive years are more prone to ankylosing spondylitis (a common form of spondylitis)?
Yes, you have heard it right.
What’s more, the constant pain impacts their efficiency and that leads to many psychological issues, too.
This happens due to a sedentary lifestyle, stress, and improper sitting posture. The worst part is that ankylosing spondylitis increases the risk of spinal fractures and osteoporosis.
But you can still heave a sigh of relief.
We are going to tell you about some of the best treatments for spondylitis that can help you live pain-free, maintain proper posture, enhance flexibility, and boost strength.
Let’s have a look at them!
What is spondylitis?
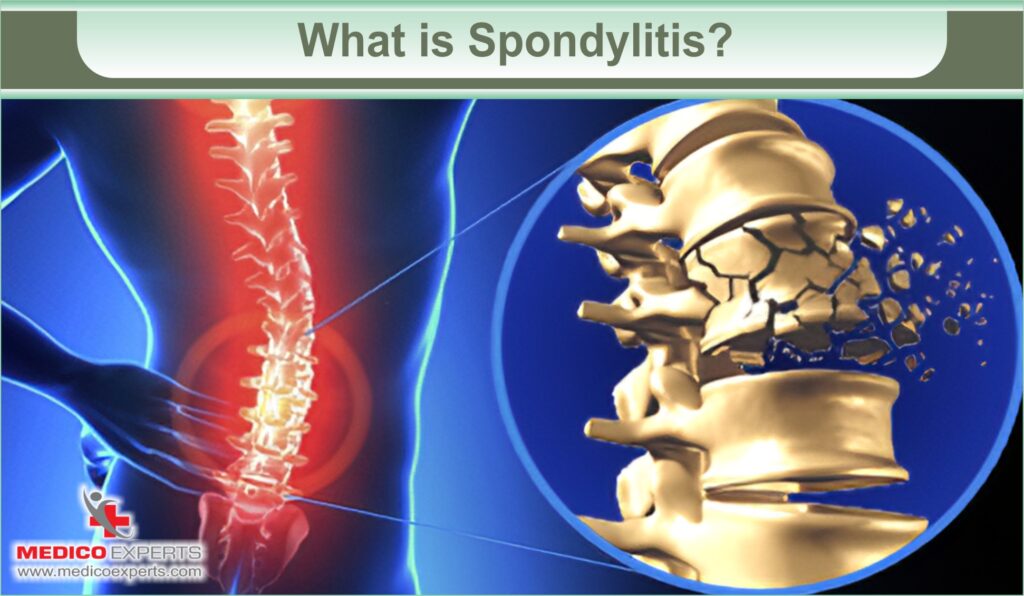
Simply put, spondylitis or spondyloarthritis is an inflammatory condition affecting your spine (especially the pelvis and lower spine), leading to pain, stiffness, and decreased mobility.
This condition often falls under the category of autoimmune diseases, with ankylosing spondylitis (an arthritic condition that results in inflammation within the spinal joints and ligaments) being one of its most common forms.
But how does spondylitis happen?
Spondylitis happens when your immune system erroneously attacks your joints and surrounding tissues and it leads to pain, excess bone formation, and bone fusion.
What are the types of spondylitis?
Spondylitis is a term that encompasses different inflammatory arthritis conditions that include:
1. Ankylosing spondylitis
Ankylosing spondylitis is a chronic inflammatory arthritis that affects your spine and sacroiliac joints, causing pain, and stiffness, and in severe cases, it can lead to fusion of the vertebrae, resulting in reduced flexibility and mobility.
2. Psoriatic arthritis
Psoriatic arthritis is a type of inflammatory arthritis that occurs in some individuals with the skin condition psoriasis. It can lead to joint pain, swelling, and stiffness, often affecting the body’s fingers, toes, and other joints.
3. Enteropathic arthritis
Enteropathic arthritis is a form of inflammatory arthritis that is associated with inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis. It can cause joint pain, swelling, and stiffness, often affecting the large joints in the lower extremities.
4. Peripheral spondyloarthritis
Peripheral spondyloarthritis is a type of spondyloarthritis that primarily affects the peripheral joints, such as those in the arms and legs, rather than the spine. It is often associated with conditions like ankylosing spondylitis and can cause joint inflammation, pain, and swelling in these peripheral joints.
5. Juvenile spondyloarthritis
Juvenile spondyloarthritis is a subset of spondyloarthritis that affects children and adolescents. It is characterized by inflammation and pain in the joints, particularly the spine, and pelvis, and may also involve enthesitis (inflammation where tendons and ligaments attach to bones) and other features similar to adult spondyloarthritis.
6. Reactive arthritis
Reactive arthritis is a type of inflammatory arthritis that typically occurs as a reaction to an infection, often in the genitourinary or gastrointestinal tract. It is characterized by joint pain, swelling, and inflammation, along with other possible symptoms such as eye or skin issues.
What are the symptoms of spondylitis?
The symptoms of spondylitis can vary depending on the type but often include these common ones:
1. Chronic Pain
Persistent pain and stiffness in the spine may worsen at night or after periods of inactivity.
2. Reduced Mobility
Difficulty bending, twisting, or performing normal movements of the spine
3. Enthesitis
Inflammation and pain where tendons and ligaments attach to the bone, commonly in the heels, elbows, or other joints.
4. Fatigue
Feeling excessively tired can be a result of chronic pain and inflammation.
5. Morning Stiffness
Stiffness in the spine and joints that is typically more severe in the morning or after periods of rest.
6. Eye Inflammation
In some types of spondylitis, like ankylosing spondylitis, eye inflammation or uveitis may occur.
7. Digestive Symptoms
In cases of enteropathic spondylitis, individuals may also experience symptoms related to inflammatory bowel diseases, such as diarrhea or abdominal pain.
8. Digestive Symptoms
You may also have a fever and lose your appetite in the early stage of spondylitis.
9. Pain in breathing
Breathing can hurt and be hard to do when your spine is bent, your lungs have inflammation or scars, or when the joints between your ribs and spine are not affected.
You need to remember that the severity and combination of these symptoms can vary from person to person.
What is the best treatment for spondylitis?

The best treatment options for spondylitis aim to lower your pain and stiffness while preventing deformities. Here are some of the treatment options:
1. Non-steroidal Anti-Inflammatory Drugs (NSAIDs)
These medications are commonly used to reduce pain and swelling associated with spondylitis. They help improve mobility and overall comfort by targeting inflammation.
2. Short-term Corticosteroids
In cases of acute flare-ups, corticosteroids may be prescribed to provide rapid relief from pain and inflammation. However, their long-term use is generally avoided due to potential side effects.
3. Tumor Necrosis Factor (TNF) Blockers
TNF blockers, a type of biological medication, are effective in reducing pain, stiffness, and swelling in spondylitis. They work by targeting specific immune system proteins responsible for inflammation.
4. Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
DMARDs are used to decrease inflammation and slow the progression of spondylitis. While they are more commonly associated with rheumatoid arthritis, some can be beneficial in spondylitis treatment.
5. Short-term Pain Relievers and Muscle Relaxants
For severe pain and muscle spasms, short-term use of pain relievers and muscle relaxants may be recommended to improve comfort and mobility while the underlying condition is managed.
6. Surgery
Surgical intervention may be necessary in certain cases to address complications of spondylitis. This can include joint replacement, spinal fusion with the placement of rods, or the removal of thickened and hardened bone to restore spinal flexibility and alignment.
7. Physical Therapy and Exercise
An integral part of spondylitis management, physical therapy, and exercise help strengthen the muscles of the back, maintain flexibility, and promote an ideal posture. These approaches are essential for managing pain and enhancing overall quality of life.
Your treatment depends on your specific condition, symptoms, and response to therapies. If you have spondylitis you need to work closely with your healthcare provider who would create a personalized treatment plan that addresses your unique needs and concerns.
Can spondylitis be treated at home?
As said above ankylosing spondylitis is the most common form of spondylitis. Though there is no cure for it, there are some home-based remedies that can help you manage the condition and alleviate the symptoms. Let’s check these remedies out:
1. Exercise
Regular physical activity is crucial for managing ankylosing spondylitis. You can do specific exercises, such as stretching and strengthening routines which can help improve flexibility and reduce pain. You can do swimming and yoga, too.
2. Posture and Body Mechanics
You need to maintain good posture and body mechanics. When you maintain a proper posture you keep the alignment of your body intact which can help reduce the stress on your spine and joints.
3. Hot and Cold Therapy
Apply heat or cold packs to affected areas. It can relieve pain and stiffness. Heat can help relax tense muscles, while cold can reduce inflammation.
4. Over-the-Counter Pain Relievers
You can also use non-prescription pain relievers like ibuprofen or naproxen. They can help manage pain and inflammation but you should use them with caution and under a doctor’s guidance.
5. Rest
Adequate rest is essential, especially during flare-ups. Ensure you have a comfortable and supportive mattress and pillows.
6. Diet
Change in diet, such as reducing inflammatory foods, can help alleviate symptoms. A balanced diet with plenty of fruits, vegetables, and lean proteins can be beneficial.
7. Stress Management
High stress levels can exacerbate symptoms. Practice relaxation techniques like deep breathing, meditation, or mindfulness to manage stress.
8. Quitting smoking
If you smoke, quitting can be beneficial since smoking has been linked to more severe ankylosing spondylitis symptoms.
9. Supportive Devices
Orthotic devices, like shoe inserts and ergonomic chairs or pillows, can help you improve comfort and posture.
Though home remedies are great ways to improve your condition, you need to constantly be in touch with your healthcare provider and opt for these remedies depending on your condition.
Summing it up
Spondylitis can be very painful, but proper treatment can help manage symptoms. It’s crucial to know your treatment options, whether it’s physical therapy, medication, lifestyle changes, or a combination.
At MedicoExperts, we understand the challenges of finding the right treatment, especially if you’re considering treatment in India. We’re here to assist you in accessing quality medical services without compromising on cost.
We connect you with top specialists and hospitals, ensuring you receive tailored care while minimizing financial strain. Your health is priceless, and we’re committed to helping you achieve a healthier life. Contact us today to start your journey towards better health.
FAQ :
Q1. Can spondylitis be cured completely?
No, ankylosing spondylitis cannot be completely cured, but its symptoms can often be managed effectively with various treatments, including medication, exercise, and lifestyle changes, allowing individuals to lead relatively normal lives.
Q2. What is the new treatment for spondylitis?
A new medicine, tofacitinib (also called Xeljanz or Xeljanz XR), has been given the green light by the FDA for treating ankylosing spondylitis in 2021.
Q3. Can walking cure spondylosis?
Walking cannot cure spondylosis, but it can help manage the condition by promoting flexibility, strengthening muscles, and reducing discomfort and stiffness associated with spondylosis. It is often recommended as part of a comprehensive treatment plan.
Q4. How long is treatment for spondylitis?
The duration of treatment for spondylitis varies from person to person and depends on the severity of the condition. In most cases, treatment is ongoing and focuses on managing symptoms and preventing further progression.
References
https://www.niams.nih.gov/health-topics/ankylosing-spondylitis/diagnosis-treatment-and-steps-to-take
https://www.ncbi.nlm.nih.gov/books/NBK551557/
https://www.sciencedirect.com/topics/medicine-and-dentistry/spondylosis



